Posterior Tibial Tendonitis
Introduction
Because we use our feet continuously, tendonitis in the foot is a common problem. One of the most frequently affected tendons is the posterior tibial tendon.
Anatomy
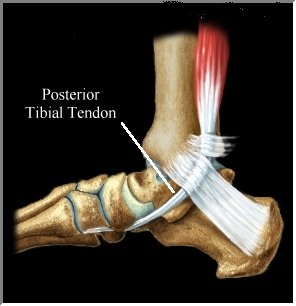
The posterior tibial tendon runs behind the inside bump on the ankle (the medial malleolus), across the instep, and at the navicular bone on the inside of the foot and into the bottom of the foot. The tendon is important in supporting the ankle and arch of the foot and helps turn the foot inward during walking. Problems with the posterior tibial tendon seem to occur in stages. Initially, irritation of the outer covering of the tendon called the paratenon causes a paratendonitis. This simply indicates that there is inflammation around the tendon as it runs through the tunnel behind the medial malleolus, (inside ankle bone). As we age, the tendon is subject to degeneration within the substance of the tendon. This creates a situation where the tendon becomes thickened and weaker, possibly to the extent that a nodule forms within the tendon. The normal arrangement of the fibers of the tendon (similar to a nylon rope) becomes jumbled, and the tendon loses strength. This condition is called tendonosis.
In many cases, the two conditions are present simultaneously. The weakened, degenerative tendon sets the stage for the possibility of actual rupture (Below) of the posterior tibial tendon. A posterior tendon rupture can be very debilitating.
(Inside view of the foot)
Symptoms
The symptoms of tendonitis of the posterior tibial tendon include pain in the instep area of the foot and swelling along the course of the tendon. In some cases the tendon may actually rupture, due to weakening of the tendon by the inflammatory process. Rupture of the tendon leads to a fairly pronounced flat foot deformity that is easily recognizable.
Diagnosis
Diagnosis of Posterior Tibial tendonitis is usually apparent on physical examination. In some difficult cases, an MRI scan may be useful to determine whether the tendon has ruptured.
Medical Treatment
Treatment of posterior tibial tendonitis begins with an orthotic devices (good supportive arch support), supportive footwear, decreased activity, and anti-inflammatory medications such as ibuprofen or aspirin.
What to expect
Most people that are compliant with wearing orthotic devices and supportive shoes achieve relief from pain to live a normal, comfortable lifestyle. Compliance is the key to avoiding surgery. Avoid unsupportive, weak shoes.
Surgery
If surgery is required, it involves removing the thickened tissue around the tendon. This is done to try and decrease the symptoms of pain and to prevent rupture of the tendon. If the tendon has ruptured, surgery may be required to either repair the ruptured tendon – or to replace it with a tendon graft. Most tears will not simply be repairable, unless they only recently occurred. Usually, another tendon in the foot, such as the tendon that flexes the four lesser toes (bends them down) is used as a tendon graft to replace the function of the posterior tibial tendon. Finally, in cases which have been neglected, and a fixed flatfoot deformity is present, a fusion (or arthrodesis) of the foot may be required.
St. Louis Sole Control orthotics and shoes to solve posterior tibial tendonitis.
9712 Watson Road
St. Louis, MO 63126 314-822-9494
Posterior tibial insufficiency, insufficient posterior tibial tendon. Posterior tibial tendon tear. Posterior tibialis tendonitis. Post tib. What is the code for posterior tibial tendonitis? The code for posterior tibial tendonitis or posterior tibial tendon insufficiency is 726.79. What is the code for orthotics for posterior tibial tendonitis? The code for orthotics for posterior tibial tendonitis is L3000.
The inside of my ankle hurts. What if the inside of my ankle hurts? The inside of my ankle swells. What if the inside of my ankle swells? What should I do if the inside of my ankle hurts? Who should I see in St. Louis if the inside of my ankle hurts? You should see a foot and ankle orthopedist. When my feet hurt I hurt all over. When your feet hurt you hurt all over. When I stand the inside of my ankle hurts. When I walk the inside of my ankle hurts. When I stand the inide of my ankle swells. When I walk the inside of my ankle swells. Who should I see about the inside of my ankle in St. Louis? The inside of my ankle hurts and swells. When I stand the inside of my ankle hurts and swells. When I walk the inside of my ankle hurts and swells. Will orthotics help the pain on the inside of my ankle? Yes. Will orthotics help posterior tibial tendonitis? Yes. What is posterior tibial tendonitis? What else is called posterior tibial tendonitis?
Posterior tibial tendonitis is an uncommon problem of one of the tendons on the inner side of the ankle. The posterior tibial muscle attaches to the back of the shin bone; the posterior tibial tendon connects this muscle to the bones of the foot. The posterior tibial tendon passes down the back of the leg, not far from the Achilles tendon, then turns under the prominence of the inner side of the ankle. The posterior tibial tendon then attaches to the bone of the inner side of the foot, just adjacent to the arch of the foot. Posterior tibial tendon problems usually occur just underneath the prominence of the inner side of ankle, called the medial malleolus. The medial malleolus is the end of the shin bone, the tibia, and the posterior tibial tendon wraps just underneath the medial malleolus. This area of the tendon is prone to problems because of a lack of blood supply. This part of the tendon exists in a “watershed zone” where the blood supply is weakest. Therefore, when the tendon becomes injured, as a result of trauma or overuse, the body has difficulty delivering the proper nutrients for healing. Symptoms of Posterior Tibial Tendonitis Most commonly, patients with posterior tibial tendonitis complain of pain in the inside of the foot and ankle, and occasionally have problems associated with an unsteady gait. Many patients report having had a recent ankle sprain, although some will have had no recent injury. As posterior tibial tendonitis progresses, the arch of the foot can flatten, and the toes begin to point outwards. This is the result of the posterior tibial tendon not doing its job to support the arch of the foot.
Diagnosis of posterior tibial tendonitis is commonly made by physical examination. Patients have tenderness and swelling over the course of the posterior tibial tendon. Usually they have weakness inverting (pointing the toes inward) their foot. Also common in patients with posterior tibial tendonitis is an inability to stand on their toes on the affected side. When the examination is unclear, or if a patient is considering surgery, an MRI may be obtained. The MRI is an effective method to detect ruptures of the tendon, and it can also show inflammatory changes surrounding the tendon. Treatment of Posterior Tibial TendonitisThe initial treatment of posterior tibial tendonitis if focused on resting the tendon to allow for healing. Unfortunately, even normal walking may not adequately allow for the tendon to rest sufficiently. In these cases, the ankle must be immobilized to allow for sufficient rest. Options for early treatment include: Shoe inserts, orthotics and arch supports, Walking boots, Casts By providing a stiff platform for the foot, shoe inserts and walking boots prevent motion between the midfoot and hindfoot. Preventing this motion should decrease the inflammation associated with posterior tibial tendonitis. Casts are more cumbersome, but are probably the safest method to ensure the posterior tibial tendon is adequately rested. Other common treatments for early stage posterior tibial tendonitis include anti-inflammatory medications and activity modification. Both of these treatments can help to control the inflammation around the posterior tibial tendon. Surgical treatment of posterior tibial tendinitis is controversial and varies depending on the extent of the condition. In early stages of posterior tibial tendonitis, some surgeons may recommend a procedure to clean up the inflammation called a debridement. During a debridement, the inflamed tissue and abnormal tendon are removed to help allow for healing of the damaged tendon.In more advanced stages of posterior tibial tendonitis, the arch of the foot has collapsed, and a simple tendon debridement may be insufficient to correct the problem. Reconstruction of the posterior tibial tendon is occasionally performed. In a reconstructive procedures, a neighboring tendon, called the flexor digitorum longus, is moved to replace the damaged posterior tibial tendon. This procedure is often combined with a bone reconstruction as well. Finally, in the most advanced cases of posterior tibial tendonitis, when the arch of the foot has become rigid, a fusion procedure is the preferred treatment.
webmaster Michael Lukowsky