COMMON FOOT DISORDERS
Planter Fasiitis – Heel Pain plantar fascitis
Plantar fasciitis is the most common foot problem and one of the hardest to overcome. The plantar fascia is a thick fibrous tissue that attaches to the heel bone (calcaneus’s) and spans across the bottom of the foot and arch and attaches to the back of the toes. It acts like a bowstring to maintain the arch of the foot.
Custom Cushioned Orthoses: For most people a custom orthotic device is necessary to maintain the long arch to keep the plantar fascia as short as possible and prevent further injury. An over the counter orthotic device may be tried for 6 to 8 weeks but if no relief is found, a custom orthoses is required.
Click here to find solutions for plantar fasciitis.
My heels hurt, what should I do? Heel pain first step out of bed hurts. Why does my heel hurt so bad? Why do both of my heels hurt? What causes heel pian? Will orthotics – inlays help heel pain? My heel hurts when I get out of bed. Do I have a stone bruise on my heel? Should I get a cortizone shot in my heel? What makes my heel hurt? I’m sick of my heel hurting. What do I do about heel pain? My foot hurts when I get out of bed. Why does my foot hurt? Why do my feet hurt? Will anything help my heels stop hurting? How do I get heel pain relief? When my heels hurt I can’t walk. I can hardly walk. Will this heel pain go away? I hate when my heels hurt. I wish this heel pain would go away. The windlass mechanism is a mechanical model that provides a thorough explanation of these biomechanical factors and stresses. The windlass mechanism describes the manner by which the plantar fascia supports the foot during weight- bearing activities and provides information regarding the biomechanical stresses placed on the plantar fascia. Heel spurs may be seen on x-ray but usually do not cause the problem. A heel spur, also called an osteophyte, is a ridge of extra bone that develops across the undersurface of the heel as the person ages. In one study 85 percent of 27 patients with plantar fasciitis had spurs; however, 46% of 79 asymptomatic controls also had spurs. In the past, surgery to eliminate the heel spur did not resolve the problem; now it is rarely done.
Could my feet cause knee pain?
Click here to find out!
Wake up Maggie I think I have somethin
My son is 9, 10, or 11 and his heels hurt why? What is making his heels hurt? This is called Sever’s disease. It is where the bones are growing faster than the soft tissue and causes the tissue that is attached to the heel to pull away from the heel, causing inflamation that causes the pain. Sever’s disease occurs in children when the growth plate (which is the growing part of the heel) is injured. The foot is one of the first body parts to grow to full size. This usually occurs in early puberty. During this time, bones often grow faster than muscles and tendons. As a result, muscles and tendons become tight. The heel area is less flexible. During weight-bearing activity (activity performed while standing), the tight heel tendons may put too much pressure at the back of the heel (where the Achilles tendon attaches). This can injure the heel and cause Sever’s disease. Sever’s disease is also called Calcaneal apophysitis. When a baby is born, most of the bones are still cartilage with only some starting to develop into bone. When the heel (calcaneus) starts to develop bone, there is generally one large area of development that starts in the center of the cartilage heel. This area of bone spreads to ‘fill up’ the cartilage. Another area of bone development (ossification) occurs at the back of the heel bone – see the x-ray to the right. These two areas of developing bone will have an area of cartilage between them – this is how the bone grows in size. At around age 16, when growth is nearly complete, these two bony areas fuse together. Sever’s disease or calcaneal apophysitis is usually considered to be due to damage or a disturbance in this area of growth. This usually happnes at ages 9, 10, 10, or 12. Why go to good feet if you can have great feet at Sole Control in St. Louis, MO?
g to say to you it s late September and my feet are really hurting me.
Metatarsalgia – Pain in the ball of the foot
Pain in the ball of the foot is normally one of two things: First and most common is Metatarsalgia. It is an inflammatory condition of the metatarsal heads. It is usually felt in the sole of the ball of the foot and sometimes feel like “walking on pebbles”. Other people feel a more diffuse vague pain, ache or burning. Some people have trouble around only one or two toes, others have it throughout the ball on one or both feet. 90% of patients with metatarsalgia are found to be wearing shoes at least one size too small. Orthotic devices and bigger shoes are usually required.
Interdigital Neuroma – Pinched nerve
Burning, tingling, aching pain radiating into two adjacent toes. It is caused from the nerve being pinched between two metatarsal bones usually from tight shoes. 90% of all neuromas are suffered by women.
Metatarsal support incorporated into custom orthotic devices; wider toe box and lower heeled footwear.
COMMON FOOT DISORDERS
Planter Fasiitis – Heel Pain plantar fascitis
Plantar fasciitis is the most common foot problem and one of the hardest to overcome. The plantar fascia is a thick fibrous tissue that attaches to the heel bone (calcaneus’s) and spans across the bottom of the foot and arch and attaches to the back of the toes. It acts like a bowstring to maintain the arch of the foot.
Custom Cushioned Orthoses: For most people a custom orthotic device is necessary to maintain the long arch to keep the plantar fascia as short as possible and prevent further injury. An over the counter orthotic device may be tried for 6 to 8 weeks but if no relief is found, a custom orthoses is required.
Click here to find solutions for plantar fasciitis.
My heels hurt, what should I do? Heel pain first step out of bed hurts. Why does my heel hurt so bad? Why do both of my heels hurt? What causes heel pian? Will orthotics – inlays help heel pain? My heel hurts when I get out of bed. Do I have a stone bruise on my heel? Should I get a cortizone shot in my heel? What makes my heel hurt? I’m sick of my heel hurting. What do I do about heel pain? My foot hurts when I get out of bed. Why does my foot hurt? Why do my feet hurt? Will anything help my heels stop hurting? How do I get heel pain relief? When my heels hurt I can’t walk. I can hardly walk. Will this heel pain go away? I hate when my heels hurt. I wish this heel pain would go away. The windlass mechanism is a mechanical model that provides a thorough explanation of these biomechanical factors and stresses. The windlass mechanism describes the manner by which the plantar fascia supports the foot during weight- bearing activities and provides information regarding the biomechanical stresses placed on the plantar fascia. Heel spurs may be seen on x-ray but usually do not cause the problem. A heel spur, also called an osteophyte, is a ridge of extra bone that develops across the undersurface of the heel as the person ages. In one study 85 percent of 27 patients with plantar fasciitis had spurs; however, 46% of 79 asymptomatic controls also had spurs. In the past, surgery to eliminate the heel spur did not resolve the problem; now it is rarely done.
Could my feet cause knee pain?
Click here to find out!
Wake up Maggie I think I have somethin
My son is 9, 10, or 11 and his heels hurt why? What is making his heels hurt? This is called Sever’s disease. It is where the bones are growing faster than the soft tissue and causes the tissue that is attached to the heel to pull away from the heel, causing inflamation that causes the pain. Sever’s disease occurs in children when the growth plate (which is the growing part of the heel) is injured. The foot is one of the first body parts to grow to full size. This usually occurs in early puberty. During this time, bones often grow faster than muscles and tendons. As a result, muscles and tendons become tight. The heel area is less flexible. During weight-bearing activity (activity performed while standing), the tight heel tendons may put too much pressure at the back of the heel (where the Achilles tendon attaches). This can injure the heel and cause Sever’s disease. Sever’s disease is also called Calcaneal apophysitis. When a baby is born, most of the bones are still cartilage with only some starting to develop into bone. When the heel (calcaneus) starts to develop bone, there is generally one large area of development that starts in the center of the cartilage heel. This area of bone spreads to ‘fill up’ the cartilage. Another area of bone development (ossification) occurs at the back of the heel bone – see the x-ray to the right. These two areas of developing bone will have an area of cartilage between them – this is how the bone grows in size. At around age 16, when growth is nearly complete, these two bony areas fuse together. Sever’s disease or calcaneal apophysitis is usually considered to be due to damage or a disturbance in this area of growth. This usually happnes at ages 9, 10, 10, or 12. Why go to good feet if you can have great feet at Sole Control in St. Louis, MO?
g to say to you it s late September and my feet are really hurting me.
Metatarsalgia – Pain in the ball of the foot
Pain in the ball of the foot is normally one of two things: First and most common is Metatarsalgia. It is an inflammatory condition of the metatarsal heads. It is usually felt in the sole of the ball of the foot and sometimes feel like “walking on pebbles”. Other people feel a more diffuse vague pain, ache or burning. Some people have trouble around only one or two toes, others have it throughout the ball on one or both feet. 90% of patients with metatarsalgia are found to be wearing shoes at least one size too small. Orthotic devices and bigger shoes are usually required.
Interdigital Neuroma – Pinched nerve
Burning, tingling, aching pain radiating into two adjacent toes. It is caused from the nerve being pinched between two metatarsal bones usually from tight shoes. 90% of all neuromas are suffered by women.
Metatarsal support incorporated into custom orthotic devices; wider toe box and lower heeled footwear.
Posterior Tibial Tendonitis – Inside ankle pain
The posterior tibial tendon runs behind the inside bump on the ankle (the medial malleolus), across the instep, and at the navicular bone on the inside of the foot and into the bottom of the foot. The tendon is important in supporting the ankle and arch of the foot and helps turn the foot inward during walking. Problems with the posterior tibial tendon seem to occur in stages. Initially, irritation of the outer covering of the tendon called the paratenon causes a paratendonitis. This simply indicates that there is inflammation around the tendon as it runs through the tunnel behind the medial malleolus, (inside ankle bone). As we age, the tendon is subject to degeneration within the substance of the tendon. This creates a situation where the tendon becomes thickened and weaker, possibly to the extent that a nodule forms within the tendon. The normal arrangement of the fibers of the tendon (similar to a nylon rope) becomes jumbled, and the tendon loses strength. The weakened, degenerative tendon sets the stage for the possibility of actual rupture of the posterior tibial tendon. A posterior tendon rupture can be very debilitating. Posterior tibial tendonitis is treated by; orthotic devices (good supportive arch support), supportive footwear, decreased activity, and anti-inflammatory medications such as ibuprofen or aspirin.
Rheumatiod Arthritis – Joint degeneration
Rheumatoid arthritis (RA) is a systemic disease that attacks multiple joints throughout the body. About 90% of the people with rheumatoid arthritis eventually develop symptoms related to the foot or ankle. Usually, symptoms appear in the toes and forefeet first, then in the hindfeet or the back of the feet, and finally in the ankles. Other inflammatory types of arthritis that affect the foot and ankle include gout, ankylosing spondylitis, psoriatic arthritis, and Reiter’s syndrome. Soft cushioned orthotics in supportive shoes is very helpful.
Pes Planus – Flat feet 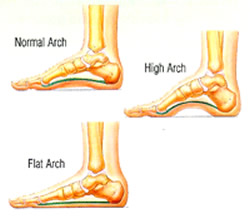
While most people with flat feet (25% of Americans) don’t have a problem, flat feet can cause disabling foot pain as well as hip pain, knee pain, shin splints, tendonitits and plantar fasciitis. In most cases a shoe insert/orthotic can be used to alleviate the symptoms of flat feet. We advise that you first see an orthopaedic surgeon in order to make sure the source of the foot pain is not serious.
Pes Cavus – High arched feet
Cavus foot is often caused by a neurologic disorder or other medical condition for example, cerebral palsy, Charcot-Marie-Tooth disease, spina bifida, polio, muscular dystrophy, or stroke. In other cases of cavus foot, the high arch may represent an inherited structural abnormality. An accurate diagnosis is important because the underlying cause of cavus foot largely determines its future course. If the high arch is due to a neurologic disorder or other medical condition, it will probably worsen. On the other hand, cases of cavus foot that do not result from neurologic disorders usually do not change in appearance. Orthotics are needed to balance foot and ankle and take pressure off the unusual high pressure areas. Some people have a disease called Charcot Marie Tooth that causes very high arches. Click here for more information.
Bunions and Hammer Toes – Bunions and hammer toes are almost always caused by short tight shoes. 90% of all bunions and hammer toes are on women. Larger deeper toe box shoes are the simplest way to solve these problems, however an orthotic device is needed to find relief.
Tarsal Tunnel Syndrome – The tarsal tunnel is a narrow space that lies on the inside of the ankle next to the ankle bones. The tunnel is covered with a thick ligament (the flexor retinaculum) and ligaments that protects and maintains the structures contained within the tunnel arteries, veins, tendons, and nerves. One of these structures is the posterior tibial nerve, which is the focus point of tarsal tunnel syndrome. Tarsal tunnel syndrome is a compression, or squeezing, on the posterior tibial nerve that produces symptoms anywhere along the path of the nerve running from the inside of the ankle into the foot. The posterior tibal nerve and blood vessel are compressed and run dwon the side of the ankle and runs down the bottom of the foot and into the toes. Tarsal tunnel syndrome is similar to carpal tunnel syndrome, which occurs in the wrist. Both disorders arise from the compression of a nerve in a confined space. This can produce burning, numbenss, tingeling and pain in the foot.
Tarsal tunnel syndrome is caused by anything that produces compression on the posterior tibial nerve, such as:
- A person with flat feet is at risk for developing tarsal tunnel syndrome, because the outward tilting of the heel that occurs with fallen arches can produce strain and compression on the nerve.
- An enlarged or abnormal structure that occupies space within the tunnel can compress the nerve. Some examples include a varicose vein, ganglion cyst, swollen tendon, and arthritic bone spur.
- An injury, such as an ankle sprain, may produce inflammation and swelling in or near the tunnel, resulting in compression of the nerve.
- Systemic diseases such as diabetes or arthritis can cause swelling, thus compressing the nerve.
Patients with tarsal tunnel syndrome experience one or more of the following symptoms:
- Tingling, burning, or a sensation similar to an electrical shock
- Numbness
- Pain, including shooting pain
When pronation is the main cause anything that can be done to stop the pronation is required. An orthotic with deep heel cups is the best way to acheive this goal.
Achilles tendonitis, also sometimes called Achilles tendinitis, is a painful and often debilitating inflammation of the Achilles tendon (heel cord). The Achilles tendon is the largest and strongest tendon in the body. It is located in the back of the lower leg, attaches to the heel bone (calcaneus), and connects the leg muscles to the foot.
The Achilles tendon gives us the ability to rise up on our toes, facilitating the act of walking, and Achilles tendonitis can make walking almost impossible.
There are three stages of tendon inflammation:
- Peritenonitis
- Tendinosis
- Peritenonitis with tendinosis
Peritenonitis is characterized by localized pain during or following activity. As this condition progresses, pain often develops earlier on during activity, with decreased activity, or while at rest.
Tendinosis is a degenerative condition that usually does not produce symptoms (i.e., is asymptomatic). It may cause swelling or a hard knot of tissue (nodule) on the back of the leg.
Peritenonitis with tendinosis results in pain and swelling with activity. As this condition progresses, partial or complete tendon rupture may occur.
Incidence and Prevalence
The overall incidence of Achilles tendonitis is unknown. The condition occurs in approximately 6 18% of runners, and also is more common in athletes, especially in sports that involve jumping (e.g., basketball), and in people who do a lot of walking.
Initial care is heel lifts to shorten the Gastrocnemius Achilles tendonitis that occurs as a result of arthritis in the heel is more common in people who are middle aged and older. If pronation is found to the cause, orthotics are indicated.
Could my feet cause back pain? Click here to find out!
Ailments of the Ankle
Achilles Tendon: Pain and swelling of the tendon at the back of the ankle either at the attachment to the heel or along the tendon
Ankle Instability: Recurrent ankle sprains and instability
Arthritis: General term for degeneration (wearing away) of the articular cartilage within a joint. Pain and swelling with standing or walking
Broken Ankle: Severe pain and swelling around the ankle after a fall, twist or other injury. Usually can t stand or walk
Sprained Ankle: Severe pain and swelling over the outside of the ankle after a twist
Posterior Tibial Tendonitis: Pain and swelling on the inside of the ankle
Peroneal Tendonitis: Pain and swelling on the outside
Ailments of the Heel
Heel Pain: Heel pain can refer to any number of conditions around the back of the foot, from Achilles tendonitis, to plantar fasciitis to a stress fracture of the calcaneus bone
Plantar Fasciitis: Inflammation of the “plantar fascia,” a thin layer of tough tissue supporting the arch of the foot (sometimes referred to as heel spurs although bony growths may not be a factor)
Rheumatoid Arthritis: Wearing away of the cartilage due to inflammation. Pain and swelling with standing or walking
Ailments of the Midfoot
Lisfranc (Midfoot) Sprain/Fracture: Severe pain and swelling of the foot in the arch and midfoot following crushing injury, fall from height, severe twisting injury or motor vehicle accident.
Lisfranc joint injuries are rare, complex and often misdiagnosed. Typical signs and symptoms include pain, swelling and the inability to bear weight. Clinically, these injuries vary from mild sprains to fracture-dislocations. On physical examination, swelling is found primarily over the midfoot region. Pain is elicited with palpation along the tarsometatarsal articulations, and force applied to this area may elicit medial or lateral pain. Radiographs showing diastasis of the normal architecture confirm the presence of a severe sprain and possible dislocation. Negative standard and weight-bearing radiographs do not rule out a mild (grade I) or moderate (grade II) sprain. Reevaluation may be necessary if pain and swelling continue for 10 days after the injury. Proper treatment of a mild to moderate Lisfranc injury improves the chance of successful healing and reduces the likelihood of complications. Patients with fractures and fracture-dislocations should be referred for surgical management.
Arthritis: General term for degeneration (wearing away) of the articular cartilage within a joint. Pain and swelling with standing or walking
Flat Feet & High Arches: Flat feet refers to a foot that has a collapsed or absent arch. High arched feet refers to a foot with an increased height of the arch. The instep of the foot is so high that only the heel, outer border and balls of the sole of the foot contacts the ground
Progressive Flatfoot: Pain along the inside of the arch and ankle. May progress to swelling, severe pain, and noticeable collapse of the arch
Rheumatoid Arthritis: Wearing away of the cartilage due to inflammation. Pain and swelling with standing or walking
Stress Fractures: Fracture without injury. Pain begins without an injry and worsens with time. Pain with walking and weight bearing
Ailments of the Big Toe
Hallux Rigidus: Arthritis of the big toe joint. Painful bone spur develops on top of joint
Bunions: Painful swelling along the inside of the big toe joint where it meets the foot. Usually accompanied by turning out of the big toe
Corns and Calluses: Hard, thickened skin cuased by pressure form improper fitted shoes
Ingrown Toenail: Pain and swelling and sometimes drainage of a toe nail or the skin where the nail meets the toe cuased from short tight shoes
Rheumatoid Arthritis:Wearing away of the cartilage due to inflammation. Pain and swelling with standing or walking
Sesamoiditis: Pain at the bottom of the big toe joint while standing or walking
Toe and Forefoot Fractures: Severe pain and swelling after a fall or injury
Ailments of the Smaller Toes
Claw Toe: Curling of one of the lesser toes. The toe curls at both joints to resemble a claw
Hammertoe: Partial curling of a lesser toe from short shoes
Morton’s Neuroma: Pain in the ball of the foot, often with numbness or burning of the toes
Metatarsalgia: Pain located under the balls of the foot
Stress fractures: Fracture without injury. Pain begins without an injry and worsens with time. Pain with walking and weight bearing
Toe and forefoot fractures: Severe pain and swelling after a fall or injury
My entire hurts a lot. It hurts when I stand or walk and continues to worsen the longer I am weight bearing.
Sole Control pedorthists in St. Louis to help with common foot disorders.
9712 Watson Rd
St. Louis, MO 63126
314-822-9494
Plantar Fasciitis-The Plantar Fascia is the thick, fibrous span of semi-elastic tissue on the sole of the foot. Often the fascia will become inflamed where it is attached at the front of the heel (usually toward the medial or inside part of the foot). There may often be a spur present with plantar fasciitis; but this is usually not the cause of the heel pain, as spurs are often found in patients with no heel pain at all. The condition is more common with pronated feet and often develops in both feet. It is common in occupations involving excessive standing and walking on hard floors. Plantar Fasciitis can be a result of some trauma such as stepping off a curb by accident; or, more likely develop over a period of time due to repeated overuse and strain without the proper support needed for an individual’s feet. If you dorsi-flex the foot (point it up toward your face) and the toes, you can usually trace the tightness and discomfort along the inner arch to the point of deep pain where the tendon attaches to the heel bone.
Plan of Action – Sometimes mild cases of Plantar Fasciitis are simple to resolve. If your Plantar Fasciitis is severe or chronic you will probably have to combine more than one type of treatment to correct the problem. COMMON FOOT DISORDERS
Planter Fasiitis – Heel Pain plantar fascitis
Plantar fasciitis is the most common foot problem and one of the hardest to overcome. The plantar fascia is a thick fibrous tissue that attaches to the heel bone (calcaneus’s) and spans across the bottom of the foot and arch and attaches to the back of the toes. It acts like a bowstring to maintain the arch of the foot.
Custom Cushioned Orthoses: For most people a custom orthotic device is necessary to maintain the long arch to keep the plantar fascia as short as possible and prevent further injury. An over the counter orthotic device may be tried for 6 to 8 weeks but if no relief is found, a custom orthoses is required.
Click here to find solutions for plantar fasciitis.
My heels hurt, what should I do? Heel pain first step out of bed hurts. Why does my heel hurt so bad? Why do both of my heels hurt? What causes heel pian? Will orthotics – inlays help heel pain? My heel hurts when I get out of bed. Do I have a stone bruise on my heel? Should I get a cortizone shot in my heel? What makes my heel hurt? I’m sick of my heel hurting. What do I do about heel pain? My foot hurts when I get out of bed. Why does my foot hurt? Why do my feet hurt? Will anything help my heels stop hurting? How do I get heel pain relief? When my heels hurt I can’t walk. I can hardly walk. Will this heel pain go away? I hate when my heels hurt. I wish this heel pain would go away. The windlass mechanism is a mechanical model that provides a thorough explanation of these biomechanical factors and stresses. The windlass mechanism describes the manner by which the plantar fascia supports the foot during weight- bearing activities and provides information regarding the biomechanical stresses placed on the plantar fascia. Heel spurs may be seen on x-ray but usually do not cause the problem. A heel spur, also called an osteophyte, is a ridge of extra bone that develops across the undersurface of the heel as the person ages. In one study 85 percent of 27 patients with plantar fasciitis had spurs; however, 46% of 79 asymptomatic controls also had spurs. In the past, surgery to eliminate the heel spur did not resolve the problem; now it is rarely done.
Could my feet cause knee pain?
Click here to find out!
Wake up Maggie I think I have somethin
My son is 9, 10, or 11 and his heels hurt why? What is making his heels hurt? This is called Sever’s disease. It is where the bones are growing faster than the soft tissue and causes the tissue that is attached to the heel to pull away from the heel, causing inflamation that causes the pain. Sever’s disease occurs in children when the growth plate (which is the growing part of the heel) is injured. The foot is one of the first body parts to grow to full size. This usually occurs in early puberty. During this time, bones often grow faster than muscles and tendons. As a result, muscles and tendons become tight. The heel area is less flexible. During weight-bearing activity (activity performed while standing), the tight heel tendons may put too much pressure at the back of the heel (where the Achilles tendon attaches). This can injure the heel and cause Sever’s disease. Sever’s disease is also called Calcaneal apophysitis. When a baby is born, most of the bones are still cartilage with only some starting to develop into bone. When the heel (calcaneus) starts to develop bone, there is generally one large area of development that starts in the center of the cartilage heel. This area of bone spreads to ‘fill up’ the cartilage. Another area of bone development (ossification) occurs at the back of the heel bone – see the x-ray to the right. These two areas of developing bone will have an area of cartilage between them – this is how the bone grows in size. At around age 16, when growth is nearly complete, these two bony areas fuse together. Sever’s disease or calcaneal apophysitis is usually considered to be due to damage or a disturbance in this area of growth. This usually happnes at ages 9, 10, 10, or 12. Why go to good feet if you can have great feet at Sole Control in St. Louis, MO?
g to say to you it s late September and my feet are really hurting me.
Metatarsalgia – Pain in the ball of the foot
Pain in the ball of the foot is normally one of two things: First and most common is Metatarsalgia. It is an inflammatory condition of the metatarsal heads. It is usually felt in the sole of the ball of the foot and sometimes feel like “walking on pebbles”. Other people feel a more diffuse vague pain, ache or burning. Some people have trouble around only one or two toes, others have it throughout the ball on one or both feet. 90% of patients with metatarsalgia are found to be wearing shoes at least one size too small. Orthotic devices and bigger shoes are usually required.
Interdigital Neuroma – Pinched nerve
Burning, tingling, aching pain radiating into two adjacent toes. It is caused from the nerve being pinched between two metatarsal bones usually from tight shoes. 90% of all neuromas are suffered by women.
Metatarsal support incorporated into custom orthotic devices; wider toe box and lower heeled footwear.
COMMON FOOT DISORDERS
Planter Fasiitis – Heel Pain plantar fascitis
Plantar fasciitis is the most common foot problem and one of the hardest to overcome. The plantar fascia is a thick fibrous tissue that attaches to the heel bone (calcaneus’s) and spans across the bottom of the foot and arch and attaches to the back of the toes. It acts like a bowstring to maintain the arch of the foot.
Custom Cushioned Orthoses: For most people a custom orthotic device is necessary to maintain the long arch to keep the plantar fascia as short as possible and prevent further injury. An over the counter orthotic device may be tried for 6 to 8 weeks but if no relief is found, a custom orthoses is required.
Click here to find solutions for plantar fasciitis.
My heels hurt, what should I do? Heel pain first step out of bed hurts. Why does my heel hurt so bad? Why do both of my heels hurt? What causes heel pian? Will orthotics – inlays help heel pain? My heel hurts when I get out of bed. Do I have a stone bruise on my heel? Should I get a cortizone shot in my heel? What makes my heel hurt? I’m sick of my heel hurting. What do I do about heel pain? My foot hurts when I get out of bed. Why does my foot hurt? Why do my feet hurt? Will anything help my heels stop hurting? How do I get heel pain relief? When my heels hurt I can’t walk. I can hardly walk. Will this heel pain go away? I hate when my heels hurt. I wish this heel pain would go away. The windlass mechanism is a mechanical model that provides a thorough explanation of these biomechanical factors and stresses. The windlass mechanism describes the manner by which the plantar fascia supports the foot during weight- bearing activities and provides information regarding the biomechanical stresses placed on the plantar fascia. Heel spurs may be seen on x-ray but usually do not cause the problem. A heel spur, also called an osteophyte, is a ridge of extra bone that develops across the undersurface of the heel as the person ages. In one study 85 percent of 27 patients with plantar fasciitis had spurs; however, 46% of 79 asymptomatic controls also had spurs. In the past, surgery to eliminate the heel spur did not resolve the problem; now it is rarely done.
Could my feet cause knee pain?
Click here to find out!
Wake up Maggie I think I have somethin
My son is 9, 10, or 11 and his heels hurt why? What is making his heels hurt? This is called Sever’s disease. It is where the bones are growing faster than the soft tissue and causes the tissue that is attached to the heel to pull away from the heel, causing inflamation that causes the pain. Sever’s disease occurs in children when the growth plate (which is the growing part of the heel) is injured. The foot is one of the first body parts to grow to full size. This usually occurs in early puberty. During this time, bones often grow faster than muscles and tendons. As a result, muscles and tendons become tight. The heel area is less flexible. During weight-bearing activity (activity performed while standing), the tight heel tendons may put too much pressure at the back of the heel (where the Achilles tendon attaches). This can injure the heel and cause Sever’s disease. Sever’s disease is also called Calcaneal apophysitis. When a baby is born, most of the bones are still cartilage with only some starting to develop into bone. When the heel (calcaneus) starts to develop bone, there is generally one large area of development that starts in the center of the cartilage heel. This area of bone spreads to ‘fill up’ the cartilage. Another area of bone development (ossification) occurs at the back of the heel bone – see the x-ray to the right. These two areas of developing bone will have an area of cartilage between them – this is how the bone grows in size. At around age 16, when growth is nearly complete, these two bony areas fuse together. Sever’s disease or calcaneal apophysitis is usually considered to be due to damage or a disturbance in this area of growth. This usually happnes at ages 9, 10, 10, or 12. Why go to good feet if you can have great feet at Sole Control in St. Louis, MO?
g to say to you it s late September and my feet are really hurting me.
Metatarsalgia – Pain in the ball of the foot
Pain in the ball of the foot is normally one of two things: First and most common is Metatarsalgia. It is an inflammatory condition of the metatarsal heads. It is usually felt in the sole of the ball of the foot and sometimes feel like “walking on pebbles”. Other people feel a more diffuse vague pain, ache or burning. Some people have trouble around only one or two toes, others have it throughout the ball on one or both feet. 90% of patients with metatarsalgia are found to be wearing shoes at least one size too small. Orthotic devices and bigger shoes are usually required.
Interdigital Neuroma – Pinched nerve
Burning, tingling, aching pain radiating into two adjacent toes. It is caused from the nerve being pinched between two metatarsal bones usually from tight shoes. 90% of all neuromas are suffered by women.
Metatarsal support incorporated into custom orthotic devices; wider toe box and lower heeled footwear.
Posterior Tibial Tendonitis – Inside ankle pain
The posterior tibial tendon runs behind the inside bump on the ankle (the medial malleolus), across the instep, and at the navicular bone on the inside of the foot and into the bottom of the foot. The tendon is important in supporting the ankle and arch of the foot and helps turn the foot inward during walking. Problems with the posterior tibial tendon seem to occur in stages. Initially, irritation of the outer covering of the tendon called the paratenon causes a paratendonitis. This simply indicates that there is inflammation around the tendon as it runs through the tunnel behind the medial malleolus, (inside ankle bone). As we age, the tendon is subject to degeneration within the substance of the tendon. This creates a situation where the tendon becomes thickened and weaker, possibly to the extent that a nodule forms within the tendon. The normal arrangement of the fibers of the tendon (similar to a nylon rope) becomes jumbled, and the tendon loses strength. The weakened, degenerative tendon sets the stage for the possibility of actual rupture of the posterior tibial tendon. A posterior tendon rupture can be very debilitating. Posterior tibial tendonitis is treated by; orthotic devices (good supportive arch support), supportive footwear, decreased activity, and anti-inflammatory medications such as ibuprofen or aspirin.
Rheumatiod Arthritis – Joint degeneration
Rheumatoid arthritis (RA) is a systemic disease that attacks multiple joints throughout the body. About 90% of the people with rheumatoid arthritis eventually develop symptoms related to the foot or ankle. Usually, symptoms appear in the toes and forefeet first, then in the hindfeet or the back of the feet, and finally in the ankles. Other inflammatory types of arthritis that affect the foot and ankle include gout, ankylosing spondylitis, psoriatic arthritis, and Reiter’s syndrome. Soft cushioned orthotics in supportive shoes is very helpful.
Pes Planus – Flat feet 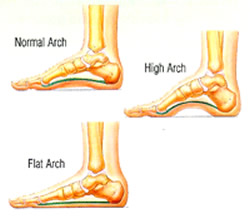
While most people with flat feet (25% of Americans) don’t have a problem, flat feet can cause disabling foot pain as well as hip pain, knee pain, shin splints, tendonitits and plantar fasciitis. In most cases a shoe insert/orthotic can be used to alleviate the symptoms of flat feet. We advise that you first see an orthopaedic surgeon in order to make sure the source of the foot pain is not serious.
Pes Cavus – High arched feet
Cavus foot is often caused by a neurologic disorder or other medical condition for example, cerebral palsy, Charcot-Marie-Tooth disease, spina bifida, polio, muscular dystrophy, or stroke. In other cases of cavus foot, the high arch may represent an inherited structural abnormality. An accurate diagnosis is important because the underlying cause of cavus foot largely determines its future course. If the high arch is due to a neurologic disorder or other medical condition, it will probably worsen. On the other hand, cases of cavus foot that do not result from neurologic disorders usually do not change in appearance. Orthotics are needed to balance foot and ankle and take pressure off the unusual high pressure areas. Some people have a disease called Charcot Marie Tooth that causes very high arches. Click here for more information.
Bunions and Hammer Toes – Bunions and hammer toes are almost always caused by short tight shoes. 90% of all bunions and hammer toes are on women. Larger deeper toe box shoes are the simplest way to solve these problems, however an orthotic device is needed to find relief.
Tarsal Tunnel Syndrome – The tarsal tunnel is a narrow space that lies on the inside of the ankle next to the ankle bones. The tunnel is covered with a thick ligament (the flexor retinaculum) and ligaments that protects and maintains the structures contained within the tunnel arteries, veins, tendons, and nerves. One of these structures is the posterior tibial nerve, which is the focus point of tarsal tunnel syndrome. Tarsal tunnel syndrome is a compression, or squeezing, on the posterior tibial nerve that produces symptoms anywhere along the path of the nerve running from the inside of the ankle into the foot. The posterior tibal nerve and blood vessel are compressed and run dwon the side of the ankle and runs down the bottom of the foot and into the toes. Tarsal tunnel syndrome is similar to carpal tunnel syndrome, which occurs in the wrist. Both disorders arise from the compression of a nerve in a confined space. This can produce burning, numbenss, tingeling and pain in the foot.
Tarsal tunnel syndrome is caused by anything that produces compression on the posterior tibial nerve, such as:
- A person with flat feet is at risk for developing tarsal tunnel syndrome, because the outward tilting of the heel that occurs with fallen arches can produce strain and compression on the nerve.
- An enlarged or abnormal structure that occupies space within the tunnel can compress the nerve. Some examples include a varicose vein, ganglion cyst, swollen tendon, and arthritic bone spur.
- An injury, such as an ankle sprain, may produce inflammation and swelling in or near the tunnel, resulting in compression of the nerve.
- Systemic diseases such as diabetes or arthritis can cause swelling, thus compressing the nerve.
Patients with tarsal tunnel syndrome experience one or more of the following symptoms:
- Tingling, burning, or a sensation similar to an electrical shock
- Numbness
- Pain, including shooting pain
When pronation is the main cause anything that can be done to stop the pronation is required. An orthotic with deep heel cups is the best way to acheive this goal.
Achilles tendonitis, also sometimes called Achilles tendinitis, is a painful and often debilitating inflammation of the Achilles tendon (heel cord). The Achilles tendon is the largest and strongest tendon in the body. It is located in the back of the lower leg, attaches to the heel bone (calcaneus), and connects the leg muscles to the foot.
The Achilles tendon gives us the ability to rise up on our toes, facilitating the act of walking, and Achilles tendonitis can make walking almost impossible.
There are three stages of tendon inflammation:
- Peritenonitis
- Tendinosis
- Peritenonitis with tendinosis
Peritenonitis is characterized by localized pain during or following activity. As this condition progresses, pain often develops earlier on during activity, with decreased activity, or while at rest.
Tendinosis is a degenerative condition that usually does not produce symptoms (i.e., is asymptomatic). It may cause swelling or a hard knot of tissue (nodule) on the back of the leg.
Peritenonitis with tendinosis results in pain and swelling with activity. As this condition progresses, partial or complete tendon rupture may occur.
Incidence and Prevalence
The overall incidence of Achilles tendonitis is unknown. The condition occurs in approximately 6 18% of runners, and also is more common in athletes, especially in sports that involve jumping (e.g., basketball), and in people who do a lot of walking.
Initial care is heel lifts to shorten the Gastrocnemius Achilles tendonitis that occurs as a result of arthritis in the heel is more common in people who are middle aged and older. If pronation is found to the cause, orthotics are indicated.
Could my feet cause back pain? Click here to find out!
Ailments of the Ankle
Achilles Tendon: Pain and swelling of the tendon at the back of the ankle either at the attachment to the heel or along the tendon
Ankle Instability: Recurrent ankle sprains and instability
Arthritis: General term for degeneration (wearing away) of the articular cartilage within a joint. Pain and swelling with standing or walking
Broken Ankle: Severe pain and swelling around the ankle after a fall, twist or other injury. Usually can t stand or walk
Sprained Ankle: Severe pain and swelling over the outside of the ankle after a twist
Posterior Tibial Tendonitis: Pain and swelling on the inside of the ankle
Peroneal Tendonitis: Pain and swelling on the outside
Ailments of the Heel
Heel Pain: Heel pain can refer to any number of conditions around the back of the foot, from Achilles tendonitis, to plantar fasciitis to a stress fracture of the calcaneus bone
Plantar Fasciitis: Inflammation of the “plantar fascia,” a thin layer of tough tissue supporting the arch of the foot (sometimes referred to as heel spurs although bony growths may not be a factor)
Rheumatoid Arthritis: Wearing away of the cartilage due to inflammation. Pain and swelling with standing or walking
Ailments of the Midfoot
Lisfranc (Midfoot) Sprain/Fracture: Severe pain and swelling of the foot in the arch and midfoot following crushing injury, fall from height, severe twisting injury or motor vehicle accident.
Lisfranc joint injuries are rare, complex and often misdiagnosed. Typical signs and symptoms include pain, swelling and the inability to bear weight. Clinically, these injuries vary from mild sprains to fracture-dislocations. On physical examination, swelling is found primarily over the midfoot region. Pain is elicited with palpation along the tarsometatarsal articulations, and force applied to this area may elicit medial or lateral pain. Radiographs showing diastasis of the normal architecture confirm the presence of a severe sprain and possible dislocation. Negative standard and weight-bearing radiographs do not rule out a mild (grade I) or moderate (grade II) sprain. Reevaluation may be necessary if pain and swelling continue for 10 days after the injury. Proper treatment of a mild to moderate Lisfranc injury improves the chance of successful healing and reduces the likelihood of complications. Patients with fractures and fracture-dislocations should be referred for surgical management.
Arthritis: General term for degeneration (wearing away) of the articular cartilage within a joint. Pain and swelling with standing or walking
Flat Feet & High Arches: Flat feet refers to a foot that has a collapsed or absent arch. High arched feet refers to a foot with an increased height of the arch. The instep of the foot is so high that only the heel, outer border and balls of the sole of the foot contacts the ground
Progressive Flatfoot: Pain along the inside of the arch and ankle. May progress to swelling, severe pain, and noticeable collapse of the arch
Rheumatoid Arthritis: Wearing away of the cartilage due to inflammation. Pain and swelling with standing or walking
Stress Fractures: Fracture without injury. Pain begins without an injry and worsens with time. Pain with walking and weight bearing
Ailments of the Big Toe
Hallux Rigidus: Arthritis of the big toe joint. Painful bone spur develops on top of joint
Bunions: Painful swelling along the inside of the big toe joint where it meets the foot. Usually accompanied by turning out of the big toe
Corns and Calluses: Hard, thickened skin cuased by pressure form improper fitted shoes
Ingrown Toenail: Pain and swelling and sometimes drainage of a toe nail or the skin where the nail meets the toe cuased from short tight shoes
Rheumatoid Arthritis:Wearing away of the cartilage due to inflammation. Pain and swelling with standing or walking
Sesamoiditis: Pain at the bottom of the big toe joint while standing or walking
Toe and Forefoot Fractures: Severe pain and swelling after a fall or injury
Ailments of the Smaller Toes
Claw Toe: Curling of one of the lesser toes. The toe curls at both joints to resemble a claw
Hammertoe: Partial curling of a lesser toe from short shoes
Morton’s Neuroma: Pain in the ball of the foot, often with numbness or burning of the toes
Metatarsalgia: Pain located under the balls of the foot
Stress fractures: Fracture without injury. Pain begins without an injry and worsens with time. Pain with walking and weight bearing
Toe and forefoot fractures: Severe pain and swelling after a fall or injury
My entire hurts a lot. It hurts when I stand or walk and continues to worsen the longer I am weight bearing.
Sole Control pedorthists in St. Louis to help with common foot disorders.
9712 Watson Rd
St. Louis, MO 63126
314-822-9494
Plantar Fasciitis-The Plantar Fascia is the thick, fibrous span of semi-elastic tissue on the sole of the foot. Often the fascia will become inflamed where it is attached at the front of the heel (usually toward the medial or inside part of the foot). There may often be a spur present with plantar fasciitis; but this is usually not the cause of the heel pain, as spurs are often found in patients with no heel pain at all. The condition is more common with pronated feet and often develops in both feet. It is common in occupations involving excessive standing and walking on hard floors. Plantar Fasciitis can be a result of some trauma such as stepping off a curb by accident; or, more likely develop over a period of time due to repeated overuse and strain without the proper support needed for an individual’s feet. If you dorsi-flex the foot (point it up toward your face) and the toes, you can usually trace the tightness and discomfort
Conservative treatments include anti-inflammatories, ice, stretching exercises, heel lifts, night splints, and orthotic devices. WEBMASTER MICHAEL LUKOWSKY ANY QUESTIONS MLUKOWSKY@SBCGLOBAL.NET